Pelvic Organ Prolapse
What is Pelvic Organ Prolapse?
Pelvic organ prolapse (POP) is a disorder where the muscles, ligaments and tissues supporting the pelvic organs become weakened or stretched. These organs including the bladder, uterus, small bowel, and rectum are allowed to migrate down and bulge into the vagina make it difficult to carry out their normal function.
Normal Pelvic Anatomy
There are three main structures that support the pelvic organs and keep them in place:
- The ligaments holding the uterus in place
- The fibrous lining in the wall of the vagina
- The pelvic floor muscles, the last line of defense that give active support through contraction
What causes a Pelvic Organ Prolapse?
- Vaginal childbirth – the stretching and straining from vaginal childbirth can affect a woman’s pelvic floor. The weight of the infant can also affect a woman’s pelvic floor.
- Pressure from obesity
- Smoking or chronic coughing from respiratory conditions
- Constipation or straining from bowel movements.
- Aging – 60 years or over women are more likely to experience pelvic disorders.
- Changes to hormones due to menopause – loss of female estrogen due to menopause can raise the risk of pelvic organ prolapse.
- Family history
- Vigorous high impact exercise
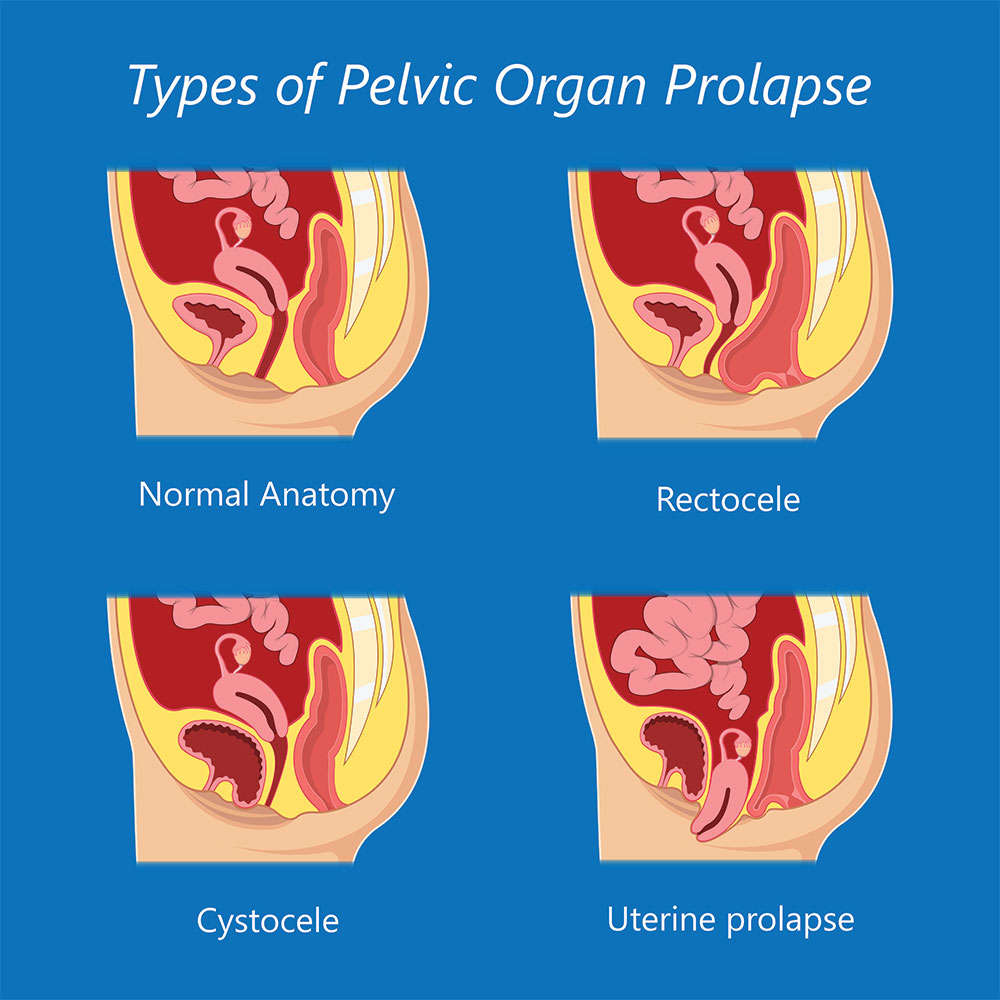
What are the Types of Pelvic Organ Prolapse?
Cystocele
A cystocele prolapse occurs when the wall between the bladder and front wall of the vagina weakens and the bladder drops or sags into the vagina. The changes to the bladder shape makes complete emptying more difficult and can lead to the body retaining urine or incomplete emptying.
Rectocele
Rectocele prolapse occurs between the back wall of the vagina and the rectum. It allows the rectum to bulge into the vagina and like cystocele, may result in difficulty emptying the bowel.
Uterine Prolapse
Uterine prolapse occurs when the uterine ligaments and pelvic floor weaken allowing the uterus to descend downward into the vagina. As uterine prolapse becomes worse the uterus may protrude out of the vagina. Uterine prolapse may affect women of any age, however it is far more common in post-menopausal women who have had at least one vaginal birth and frequently occurs with a cystocele or rectocele.
What are the Symptoms of Pelvic Organ Prolapse?
Symptoms of Pelvic Organ Prolapse include:
- Feeling of heaviness around the lower abdomen and genital area
- Feeling or appearance of a bulge or lump in or coming out of the vagina
- Pressure of the pelvis that gets worse with standing and other day to day activities
- Pressure, aching or discomfort in the pelvis, especially during sex or physical activity
- Feeling of looseness in the vagina – inability to keep a tampon in or decreased tone during sex
- Urine leaking or urine retention
- Difficulty with bowel movement
- Recurrent urinary tract infections
Prevention and Treatment of Pelvic Organ Prolapse
To reduce your risk of uterine prolapse, try to:
- Perform pelvic floor exercises regularly. These exercises can strengthen your pelvic floor muscles — especially important after you have a baby.
- Always brace and engage. While its important to do pelvic floor exercises, it’s even more important to train using them in real life situations. Conciously engaging your pelvic floor before picking up a heavy object, jumping or coughing can help to protect against prolapse or prevent further stretching.
- Treat and prevent constipation. Drink plenty of fluids and eat high-fiber foods, such as fruits, vegetables, beans and whole-grain cereals.
- Avoid heavy lifting and lift correctly. When lifting, use your legs instead of your waist or back.
- Control coughing. Get treatment for a chronic cough or bronchitis, and don’t smoke.
- Avoid weight gain. Talk with an Accredited Exercise Physiologist or doctor to determine your ideal weight and get advice on weight-loss strategies, if you need them.
- Modify activities. If you’ve previously been a runner or played netball it might be helpful to look at activities that place less force on your pelvic support structures. Cycling or swimming can be great alternatives to running for cardio. Weight training is still possible with good technique, however you may need to train with lighter resistance.

Prognosis
Remember every body is different and in some cases the prolapse may be more advanced. If this is the case there are some additionmal options available.
A pessary is a device that can be prescribed and fitted by a womens health physiotherapist. It acts a little like a brace in that it splints the wall of the vagina and provides extra support to improve the alignment of the pelvic organs. It can make emptying the bladder and bowel easier and reduce the heaviness or dragging sensation you may be experiencing.
In some cases, conservative treatment may not be enough and surgery may be required to repair damaged tissues or place additional supports within the pelvis however this can be complicated and challenging so trying conservative methods with your physiotherapist to guide you is a good first alternative.
How to Make an Appointment
Making an appointment at our Physiotherapy clinics is as easy as booking online for your nearest Brisbane based Activate Physiotherapy clinic in Stafford or Gumdale.
